New resus rooms, new trauma bay........time to get yourself up to date with trauma care in 2015!
St Emlyns and the College FOAMed Network have joined forces to make its easy for you. The following blog and podcast are also available on www.cemfoamed.co.uk/portfolio/top-10-trauma-papers-2014-15/
Top 10 trauma 2014 15 from Simon Carley
I was lucky enough to team up with Simon Laing from the RCEM FOAMed network to podcast on the top 10. We are jointly publishing this on both sites so please have a listen, follow the references and if you agree or disagree with my opinions please let me know in the comments section, on twitter or on facebook. So with that in mind, in no particular order and with a selection process entirely based on ‘stuff I like’ here’s the top 10.
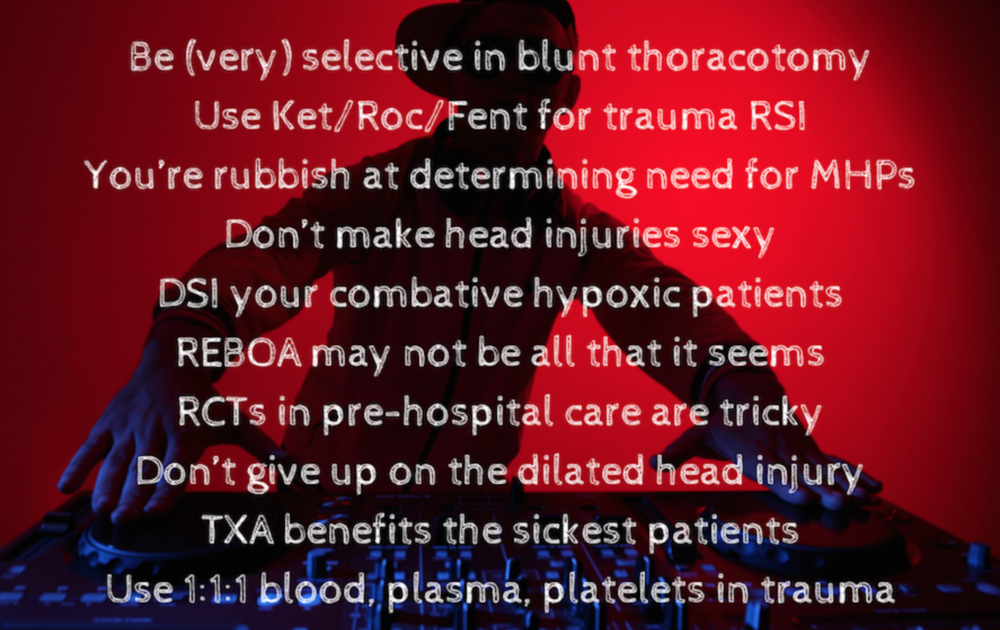
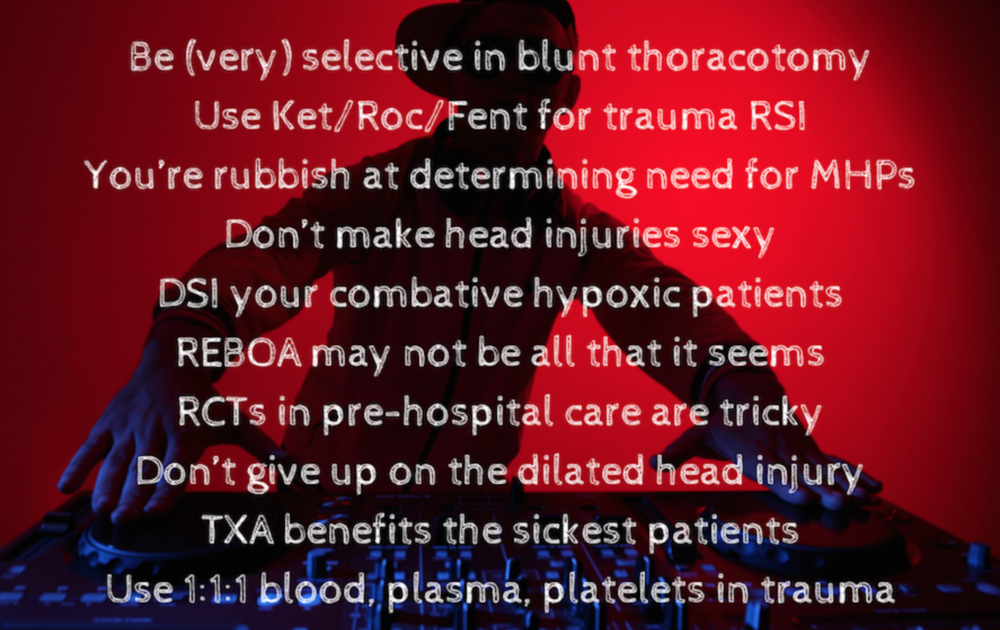
Number 1. PROPPR trial
We’ve talked about this on the St.Emlyn’s site already. This is an RCT of 1:1:1 vs. 1:1:2 (platelets/FFP/blood). It’s a well conducted trial relevant to our trauma patients who need blood. The bottom line? Use 1:1:1 it’s statistically just as good, and there is a suggestion that this trial is under-powered to demonstrate superiority of 1:1:1. Read more from Salim at REBEL EM and listen to Ken and Salim discuss it at SGEM.
Number 2. Progesterone in major head injury
Again a paper we’ve reviewed here at St.Emlyn’s. A well designed RCT that promised much on the management of patients with GCS 4-12 significant head injury. The bottom line? No benefit to progesterone infusions in these patients. So it’s a no to progesterone in the real world despite promising animal data.
Number 3. Fixed dilated pupils in head injury – What’s the prognosis?
Arguably better than you thought! A small systematic review that gives us the real world outcome data for head injured patients with fixed dilated pupils. The headline here is that those with an extradural and fixed dilated pupils have a >50% chance of a good neurological recovery. Please, please, please aggressively manage these patients and avoid any nihilism as a result of this pupilary sign. Don’t forget to sign up to one of the authors, Mark Wilson’s,GoodSAMApp too.
Number 4. How good is REBOA?
There’s lots of interest in REBOA at the moment and I get that. It’s exciting and pathophysiologically it makes sense for patients with exsanguinating lower body bleeding. It’s fairly new to the UK and centres such as London HEMS are instituting it carefully and systematically with good training and audit processes. What of the rest of the world though? Well others, such as the Japanese, have been doing this for some time and in a registry based paper they compared patients receiving REBOA with matched controls who did not. They found a much higher mortality (75%)in those receiving REBOA. There are many reasons why this may be and it’s not reason to NOBOA (get it ?!?)but it does mean we need to carefully evaluate how we impliment it, who gets it and what happens to them. If 99% were going to die anyway but by using REBOA the Japanese managed to improve it to 75% that’s a positive result. We just don’t know yet, but we may do soon as the AORTA trial is ongoing in the US. More on REBOA at LITFL, EMCRIT and RCEMFOAMed.
Number 5. The HIRT trial. An RCT of Physician PHEM for head injured patients.
This trial is worth a read as it’s big, expensive, ambitious and controversial. An RCT of physician staffed helicopter vs. ground paramedics for the treatment of head injured patients in Sydney. The trial reports an improved outcome for GCS<10 patients, no difference for GCS <14. However, lots of controversy and worth reading comments on this from luminaries such as Karel Habig in Sydney, with some real concerns about intention to treat vs. delivered therapies and interventions. You should also read the authors own reflections on prehospital research here. Whatever you make of this study if you are interested in prehospital trauma research it’s well worth reading the paper and all the controversies that surround it.
Number 6. DSI for the hypoxic patient
A bit of a cheeky one this as an observational study on the use of Delayed Sequence Intubation. Sadly only 2 trauma patients in the study so arguably should not be here. However, as a proof of concept for combative, hypoxic patients it may be helpful. More on DSI here. Arguably we’ve been doing it for years but previously never had a name for it…….
Number 7. Gestalt in predicting major bleeding in trauma patients.
When I’m in the resus room as a trauma team leader I often wonder whether or not to activate the major haemorrhage protocol. Sure, for those patients who are hosing blood out of every orifice (new and traditional) then sure it’s easy. Similarly for those patient who are completely fine with no apparent on going bleeding it’s easy (don’t do it). However, there are a number of patients that I see where it’s a tough call. I’ve often thought that I’m just not very good at this, I’ve flirted with objective scores and worried that others are better than I. The bottom line is that despite many years of trauma management I still struggle, so I was interested to see this paper on clinician ‘Gestalt’ in the resus room with reference to whether patients need MHPs. The bottom line is that clinicians are poor at deciding which patients are going to require major haemorrhage and so are the objective scores. Gestalt may not be that great. As a Trauma Team Leader this tells me that I must be vigilant and constantly reassess the need for 1:1:1 resuscitation.
Number 8. Standardising drugs for trauma RSI.
I chose this paper as it’s an issue in Virchester. We do a lot of RSI in our resus and it’s noticeable that there is much variation in drug use. In contrast those I really respect as resuscitationists in PHEM have adopted standardised approaches to drug use. KSS looked this and compared an old regime (etomidate plus sux) vs Ket/Fent/Roc and found the latter to give better views and cardiac stability. Although a before/after historical trial it fits with my belief that that Fent/Ket/Roc is a good regime to use as a baseline protocol for trauma (ED) RSI.
Number 9. TXA in severely injured patients.
If you follow St.Emlyn’s you will know that we are big fans of TXA. However, the world (mostly US/Aus) don’t always agree. CRASH-2 was a multicentre, multinational study that involved different types of trauma systems. Some in what they perceive to be ‘advanced’ trauma systems claim that TXA would not work for them. I recently experienced this in the US where this trial (observational crap) was used to refute CRASH-2. Honestly? I don’t get it, but the bottom line is that patients may be losing out across the world as a result of the lac of adoption of TXA.
Number 10. Lastly Thoracotomy in blunt trauma.
I have been taught for many years that there is no role for thoracotomy in blunt trauma. I can remember waiting to receive a patient with pre-alerted traumatic cardiac arrest in Virchester, I’d briefed the team and we were prepped when just before the patient arrived the consultant surgeon burst through the door and immediately shouted to all present ‘The one thing we are not ******** doing is a thoracotomy’. It was an interesting moment…….., and some education took place….. Anyway, it reflects the dogma that there is no role for thoracotomy in blunt trauma, but is that right? Well perhaps not. In this systematic review there are some survivors, albeit just 1.5% neurologically intact. Is that a futile therapy? Perhaps not and if your patient has a potentially survivable injury and arrests in front of you it may be worth a go. The authors outline an algorithm for patient selection. Read more at EMLitofNote.
So there you go. Ten papers in a fairly lean year for high quality science, but much to think about and a few that may really change practice in the resus room. As with everything on St.Emlyn’s don’t take my word for it. Follow the links, listen to the podcast, read the papers and make up your own mind .
vb
S
References & Links
1. Transfusion of Plasma, Platelets, and Red Blood Cells in a 1:1:1 vs a 1:1:2 Ratio and Mortality in Patients With Severe Trauma The PROPPR Randomized Clinical Trial.
JAMA. 2015;313(5):471-482. doi:10.1001/jama.2015.12
2.Very Early Administration of Progesterone for Acute Traumatic Brain Injury. N Engl J Med 2014; 371:2457-2466
3. Prognosis of patients with bilateral fixed dilated pupils secondary to traumatic extradural or subdural haematoma who undergo surgery: a systematic review and meta-analysis. Emerg Med J doi:10.1136/emermed-2014-204260
4. Survival of severe blunt trauma patients treated with resuscitative endovascular balloon occlusion of the aorta compared with propensity score‐adjusted untreated patients. Journal of Trauma and Acute Care Surgery: April 2015 – Volume 78 – Issue 4 – p 721–728 doi: 10.1097/TA.0000000000000578
5. The Head Injury Retrieval Trial (HIRT): a single-centre randomised controlled trial of physician prehospital management of severe blunt head injury compared with management by paramedics only. Emerg Med J doi:10.1136/emermed-2014-204390
6. Delayed Sequence Intubation: A Prospective Observational Study. Ann Emerg Med. 2015 Apr;65(4):349-55.
7. Clinical gestalt and the prediction of massive transfusion after trauma. Injury Volume 46, Issue 5, May 2015, Pages 807–813
8. Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia. Critical Care 2015, 19:134
9. Tranexamic Acid Use in Severely Injured Civilian Patients and the Effects on Outcomes: A Prospective Cohort Study. Annals of Surgery: February 2015 – Volume 261 – Issue 2 – p 390–394
10. To be blunt: are we wasting our time? Emergency department thoracotomy following blunt trauma: a systematic review and meta-analysis. Ann Emerg Med. 2015 Mar;65(3):297-307.e16